One reason nobody wants to live in a nursing home? They’re terribly designed
The stark difference between an aged-care “home” and a real home has been laid bare by the COVID pandemic.
Residential aged-care buildings are often institutionally designed, even if they have the appearance of a hotel. Think long corridors, vast dining rooms, nursing stations, and bland corporate furnishings. These design choices support a model of care underpinned by cost efficiencies rather than real people’s rhythms of daily life.
So, how can we make aged-care facilities feel more like home while keeping them pandemic-safe?
Designing a more home-like nursing home
Residential aged-care facilities are deeply restrictive environments; some have been compared to prisons. During the pandemic, things were made even worse as residents were denied the right to leave their rooms or have visitors. For many residents, it must have felt like the prevention was worse than the disease, as physical and psychological health declined markedly in imposed isolation.
Hotel-like residential aged-care rooms are no place to be for long periods without the company of others. Some may look like luxury resorts, but residents are still “incarcerated.” Often, residential centers are more like a “container” than a home; a container that dispenses shelter, food, and medical care.
So, what might we do differently in the post-pandemic era?
To try to answer this question, we held a collaborative design workshop involving architects and stakeholders, including managers from the residential aged-care sector. We sought to visualize design ideas using three existing not-for-profit residential sites as testing grounds.
We asked the group to ponder: What makes a home “home-like”? And how does that differ from the environment at an aged-care center?
Three key ideas emerged, all of which could help a facility feel more like a home while also reducing the impact of future pandemics.

Become part of the neighborhood
Residential aged-care facilities are often walled and gated enclaves set apart from the surrounding community. Residents are secluded in wards, not part of the natural ebb and flow of the community. A home, on the other hand, is usually directly connected to the outside world.
Embedding indistinguishable residential aged-care households in the heart of an active community would add to the broader social and physical fabric and build support networks. In practice, this could mean opting for smaller buildings that look similar to surrounding buildings, rather than the large and imposing structures we have today.
It could mean offering a wide range of housing choices, from houses to apartments, and softening wall and gate barriers so residents could easily connect with everyday community life.
Create ageless communities
Our group took inspiration from the urban design concept known as the “five-minute community,” where everything is a short walk away.
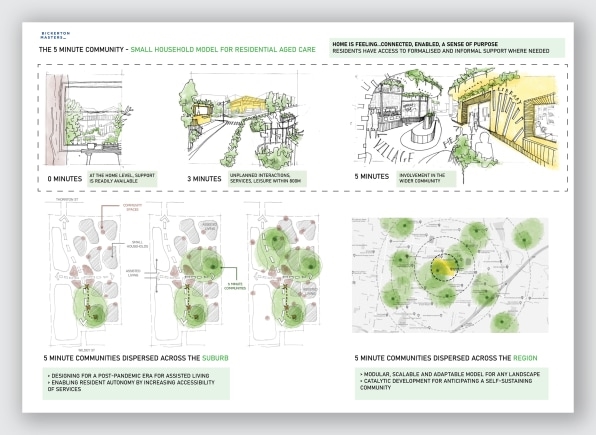
[Image: Bickerton Masters]
We imagined designs that allow for self-sufficient small households of up to eight residents, with different generations living on the same street. “Ageless” communities like this allow for generations to interact, incidentally or deliberately.
Residents could easily adjust the level of support needed over time, while staying at home. Intensive rehabilitation could be delivered in the home or nearby. For example, people who have had a fall could access rehabilitation and restorative services in the local area.
We also looked for ways to take advantage of existing spaces in the community rather than constructing new aged-care facilities that are set apart.
Big isn’t always better
Small-home models deliver an antidote to isolation and the spread of airborne respiratory infection.
Smaller stand-alone buildings are less dependent on centralized air-circulation systems and can deliver strategies to reduce infection transmission by making sure all rooms have access to fresh air and natural ventilation.
Also, smaller households can quarantine without the need to lock down an entire large facility.
Living, not just existing
Entrenched approaches to residential aged-care design assumes residents can do little independently. An unquestioning focus on inabilities further disempowers: “care” is done “to” or “for” a resident in a “facility.”
For example, residential aged-care meals are generally preprepared and eaten in a large-scale room with many others (including strangers).
At home, by contrast, people decide what, when, and where to eat. The small-home approach in five-minute communities would allow, for instance, people of different generations to cook together, or for a younger person to cook for an older person while also learning new skills.
Designs that acknowledge older people’s knowledge and skills can help allow for such interactions to occur.
When workshop participants challenged their own expectations, they envisioned design concepts emphasizing living, not just existing, until end of life.
The residential aged-care crisis is escalating, and structural and cultural change is desperately needed. It’s time to rethink these physical environments with peoples’ fundamental needs at the heart of design.
Rosemary Kennedy is an adjunct professor of architecture and urban design at Queensland University of Technology; Laurie Buys is an honorary professor at The University of Queensland. This article was republished from The Conversation under a Creative Commons license. Read the original article.
(50)



