Artificial skin transplants could be used to treat diabetes
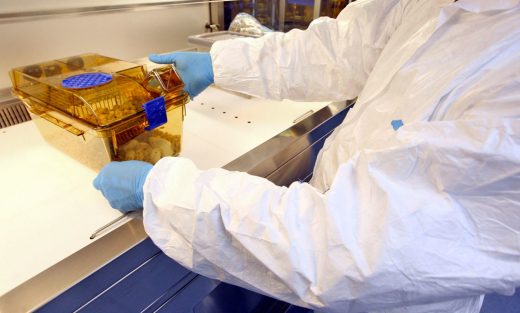
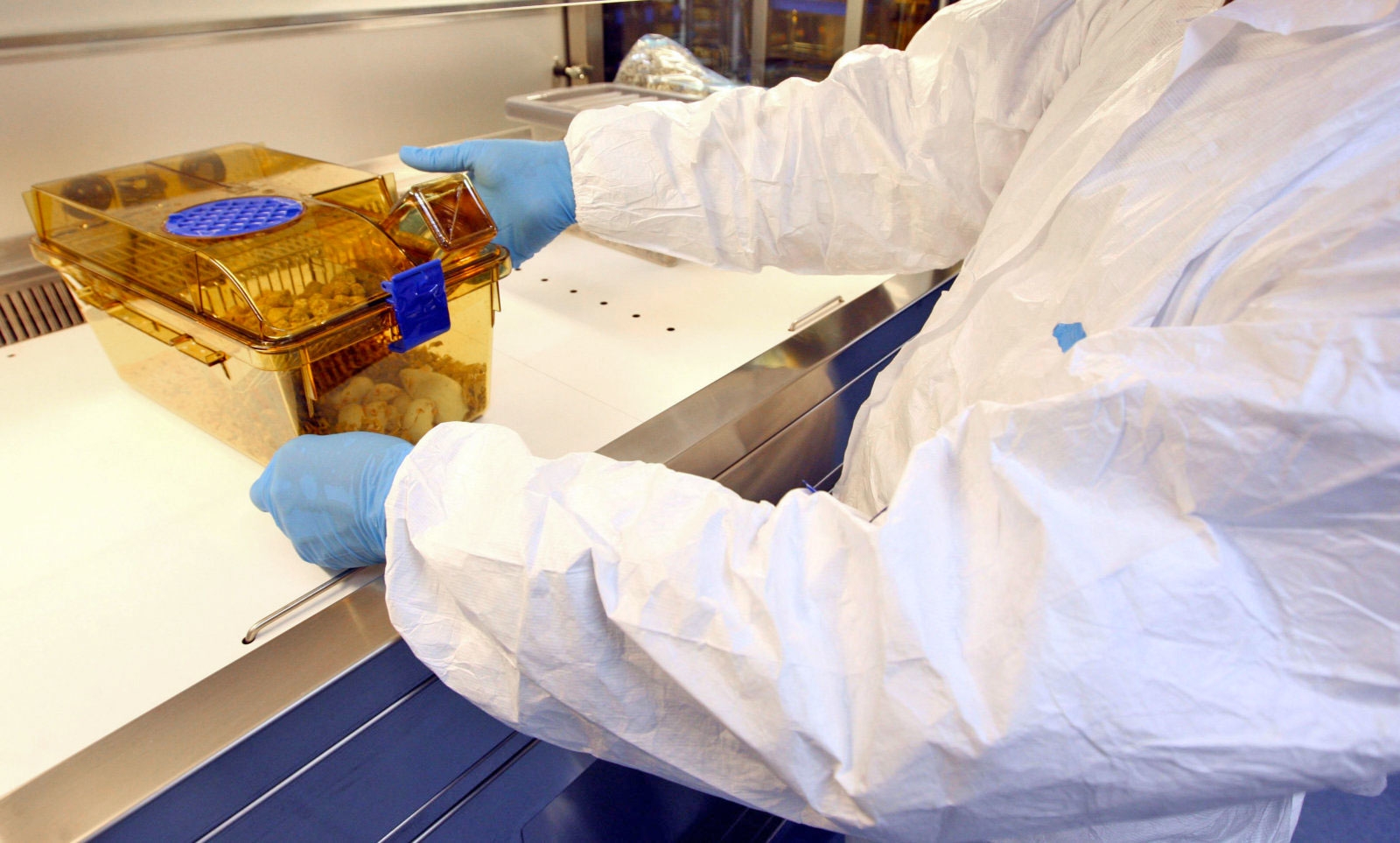
Skin grafts made using CRISPR gene editing are preventing mice from developing diabetes, and scientists claim they could prove beneficial for humans too. In a proof-of-concept study, researchers at the University of Chicago edited stem cells from newborn mice to controllably release glucagon-like peptide 1 (GLP-1). This is the hormone that stimulates the pancreas to produce insulin while maintaining healthy levels of blood glucose. The genetically modified skin grafts were then given to mice that were fed high-fat diets to induce obesity. These mice saw a reverse in insulin resistance and gained around half as much weight as those not given the grafts.
Obesity is one of the main risk factors that can cause type 2 diabetes, with high insulin resistance leading to the development of the condition. According to the study’s senior author, the inexpensive nature of growing human skin from stem cells means the treatment could work for people with the condition.
Artificial skin has been used to treat burn patients for decades. But as the the process has developed, to the point where skin can now be grown in a lab, researchers have sought other clinical uses for the treatment. However, a major hurdle that kept holding them back was a lack of test subjects. Until now, stem cell-generated skin transplantation has only been shown to work on mice with weakened immune systems. This latest study marks a breakthrough, as it is the first time the process has worked long-term on wild mice. The researchers claim they can now look into using different gene-edited grafts to treat other diseases.
“We didn’t cure diabetes, but it does provide a potential long-term and safe approach of using skin epidermal stem cells to help people with diabetes and obesity better maintain their glucose levels,” said senior author Xiaoyang Wu.
(23)