Atlanta announces new HIV testing pilot aimed at reducing high infection rates
Months before the federal government started shipping out its first batch of at-home COVID-19 tests, many local municipalities had already taken the initiative. In September 2021, Atlanta’s Fulton County started sending out free kits, made by a diagnostics company called Quidel, specifically to zip codes that were home to populations with high COVID-19 rates, large numbers of essential workers, or lower-than-average vaccine uptake.
Once adopted, at-home testing in general proved to be not only convenient and quick but also reliable when used correctly, and in many cases it helped combat issues around accessibility and privacy.
This pandemic diagnostics lesson is now being harnessed to improve testing and treatment of sexually transmitted infections (STIs). Fulton County, which has one of the highest HIV infection rates in the country and is home to Atlanta, is partnering with remote diagnostics startup Ash Wellness to deliver free test kits to residents to self-swab for STIs.
While other similar STI diagnostics partnerships exist around the U.S., this pilot is different in a critical way: The county’s health department, not the company, is responsible for community outreach. That helps ensure that the program is tailoring engagement to meet the needs of its population, an approach that proved effective in COVID-19 vaccine uptake. Because test results are automatically reported to the Fulton County Board of Health’s communicable disease specialists, health officials will follow up with treatment advice for residents who test positive, navigating them to the care they need.
Georgia has consistently grappled with one of the highest rates of new HIV infections in the U.S., gradually rising from the nation’s eighth-highest rate in 2007 to the fifth-highest in 2015. (The state stopped reporting its ranking that year, but its infection rate has only grown since then.)
In 2020, 24.7 per 100,000 of people ages 13 and older were diagnosed with HIV, according to the Georgia Department of Health. Of those infections, 84% were attributed to male-to-male contact, and 71% of new diagnoses were among Black people. Of Georgia’s 18 public health districts, Atlanta’s Fulton County had the highest rates, along with neighboring DeKalb.
In response to the high infection rates, the Fulton County Board of Health is using a portion of its annual funds from the Centers for Disease Control and Prevention (CDC) to launch an at-home testing pilot, initially dedicating 700 kits for distribution, at a cost to the agency of approximately $100 per kit. Residents will be able to log into a portal on the county’s StopHIVATL website and sign up for a free kit. (The health board and some community organizations that serve unhoused residents also will have test kits available on-site for those who might not have an address.)
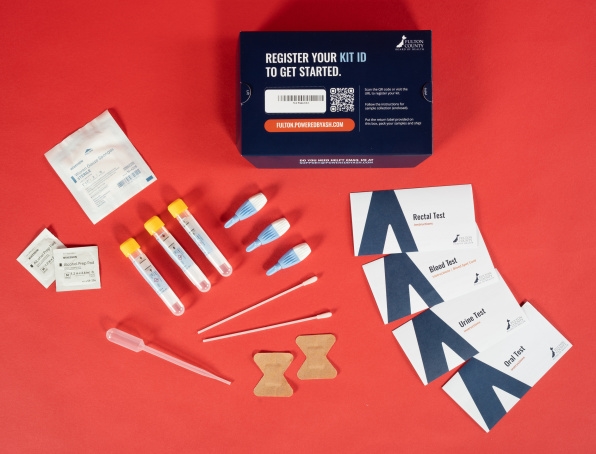
Depending on specific needs, the county can supply blood spot tests for HIV and syphilis, as well as urine tests, and throat and rectal swabs to test for chlamydia and gonorrhea.
“We ask what body parts the individual is using sexually, then determine what type of test would be best for them,” explains Joshua O’Neal, sexual health program director for the Fulton County Board of Health. Residents then send their samples to a diagnostics lab, which expects to turn results around within three to five days of receipt.
The tests are produced by Ash Wellness, which partners with public systems, universities, and digital health companies across 50 states. The partners hope to bypass the stigmas and embarrassment that people may feel around STI testing, which may discourage them from testing at public clinics. The at-home option is also beneficial for undocumented immigrants, and for people who can’t take time off work, who don’t have a doctor, or who generally don’t have faith in established medical systems.

The CDC reported that the U.S. had a 17% drop-off in HIV diagnoses in 2020 compared to 2019, likely due to COVID-19. Pandemic or not, “people are still having sex, and they’re having lots of it,” says Kyle Waters, cofounder and chief product officer at Ash Wellness, but they’re not testing because of the risk of getting COVID-19 in crowded clinic environments. As for the county’s health system, O’Neal says, COVID-19 became the overwhelming priority. “We didn’t have the same capacity to do the HIV work that we needed to do.”
During the pandemic, people have also become accustomed to testing themselves. O’Neal says that when it comes to STI testing, which can be sensitive due to rectal swabs, he now prefers doing it himself. “The last time I got it done, the doctor had no clue what they were doing,” he says. “It was totally uncomfortable.”
Ultimately, Fulton County officials decided to pursue this pilot model because it relies heavily on patient outreach, which during the pandemic became a critical part of keeping people connected to medical care. Community messaging from a trusted source proved an important factor in persuading populations to get the COVID-19 vaccine. Now, in providing guidelines for STI testing, Fulton County publishes instructions, with audio and video components, on its website and across its social media platforms, in a language that is familiar and accessible—whether, O’Neal says, that “language” is Spanish, or in a Southern accent, or related to the queer experience.
The county will also be responsible for following up with a patient who gets a positive result. The Board of Health will call the individual to direct them to treatment options, depending on their insurance and preferences. This approach differs from some existing public-private testing partnerships, in which the local government hands off the healthcare process to its corporate partner, including one in Colorado that partners with diagnostics company Binx Health. Another in Southeast Georgia, with OraQuick, puts the burden on the patient to report results and find treatment, which can lead to underreporting.
“Just partnering with somebody as random as a faceless tech corporation is not going to be what works,” Waters says.
O’Neal hopes that this system can inspire other municipalities’ testing procedures, and he says that Georgia is already willing to expand the process statewide if the pilot is successful. It’ll come down to demand and uptake, but things look promising: There have been 65 orders already, even before the formal pilot announcement.
Whatever the outcome, O’Neal sees the urgency of rolling out the program now, while people are naturally acclimated to the new pandemic-era way of doing things. “Now’s the time to ride that momentum,” he says, “instead of losing it and trying to rebuild entirely.”
Fast Company , Read Full Story
(18)



