Cancer Cures Could Already Exist In Big Data
“Reuse, and recycle” is a famous saying of the environmental movement, but cancer researchers might learn a thing or two from that mantra as well.
That’s the gist of several recommendations that came out today from a blue-ribbon panel set up by the White House as part of President Obama’s Cancer Moonshot program. Its audacious goal is to move the needle closer to a cure and achieve a decade’s worth of progress in five years.
Today’s full report, one of three that will come out this year, features 10 recommendations. They include lots of new research, such as on immunotherapy and causes of childhood cancers, as well as finding ways to minimize side effects of cancer treatments.
But pooling data is perhaps the biggest component, weaving its way through several recommendations. It would start with patients, through a network that lets them preregister online as candidates for clinical trials. In the process, they would submit cancer tissue samples to be genetically sequenced.
Each of the reports will include proposals for how to tackle cancer research and cures. Members of this panel included mainly university and hospital researchers, as well as some government officials and private-sector execs. Given the laudatory fanfare today’s report received, it’s a safe bet that it won’t fly in the face of the upcoming other two reports—one from Vice President Joe Biden, who heads the Moonshot effort, and another from a White House task force of government departments and agencies.
Reusing And Recycling Patient Info
Instead of having to recruit participants from scratch, researchers doing clinical trials would already have a pool of willing volunteers to pull from. The online network also helps involve the majority of cancer patients who don’t live close to the elite research institutes that do most clinical studies. This registry might look like an existing program run by the Broad Institute and the Dana-Farber Cancer Center in Boston, which uses social media to recruit volunteers. It also resembles the specialized registries created by PatientCrossroads for more than 60 conditions, such as Lyme disease, kidney cancer, and obscure disorders like hypertriglyceridemia (high fat levels in blood).
The most ambitious—and potentially headache-inducing—proposal is a recommendation to build a “national cancer data ecosystem.” It would link up patient databases from around the country, such as those kept by hospitals, universities, nonprofits, and government institutes so that researchers could access information like biopsy reports beyond those at their own institutions.
In a world where just transferring medical records from one doctor to the next is an ordeal, linking massive, not-yet-compatible databases is a monster undertaking. Confidentiality could also be a concern. Would every patient have to give consent to have their data made available to other researchers (even if it’s anonymous)? Then there are egos: Institutions that spend years and fortunes collecting data often resist sharing it.
There are precedents, though. For instance, the U.S. National Institutes of Health (NIH) has hooked up with a half-dozen hospitals and universities to form the Undiagnosed Disease Network, which pools data on super-rare conditions (like those with just a half-dozen sufferers), for which every patient record is a treasure to researchers.
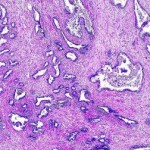
An example of recycling is a proposal to “mine” past patient records to see what worked. Biobanks hold tumor samples for patients who have already gone through different kinds of cancer care, such as chemotherapy or immune system treatments. Some are successful, some aren’t. Some treatments work for a while, then stop working. By comparing how a patient fared to the details of their tumor—like specific mutations and proteins present, researchers might get a better sense of why certain treatments will or won’t work on certain tumors.
Bringing Kids Into The Mix
Cancer is often thought of as a disease for older people. It’s also the leading cause of death from disease among children in the U.S. Childhood cancer is one of the areas that needs a lot of fresh research, because kids’ tumors don’t look like those of adults. They typically don’t have as many genetic mutations, but they do have fusion oncoproteins—molecules formed when garbled genetic code combines what should be two separate proteins into one malformed Franken-molecule. Researchers are just beginning to figure out how these proteins form.
“That they even highlighted pediatric cancer in itself is a huge leap,” says Danielle Leach of the child cancer-focused St. Baldrick’s Foundation, who took part in the panel’s pediatric working group. “Our needs are different and unique, and we need to look at them through a different lens than adults.”
Pediatric cancer research is especially dependent on government funding, says Leach, whose son Mason died at age 5 from a brain tumor. There aren’t nearly as many child cancer patients as there are adults, which makes pharma companies less interested in developing treatments. “We don’t have the patient population for a billion dollar drug that’s only going to go into a thousand kids,” she says.
As in many cases, government funding could be the real burden for Obama’s cancer plans. Back in February, the president proposed spending an extra $1 billion on the Moonshot program. Meanwhile, Congress has spent most of the year arguing over funding for the clear and present danger of Zika—with the latest impasse happening in the Senate just this week.
“Even if we don’t get any of the appropriations, we will be able to begin some of the implementation,” says Dinah Singer, acting deputy director of the National Cancer Institute (part of NIH), in a meeting with journalists. “But the rate obviously would be greatly enhanced with the kind of funding that the vice president has been talking about.”
Getting money is especially shaky, given that this request comes from a lame duck president whose party doesn’t control Congress. “I think there’s a lot of commitment to cancer research and there’s a lot of champions on both sides of the aisle for health care research,” says Leach. “But I think how you get there and how you fund it—there are fundamental differences.”
Fast Company , Read Full Story
(22)