Data show telehealth is more of a luxury good right now
By Sanjula Jain
With the recent passage of the omnibus spending bill, which, in part, addresses telehealth, Congress is expected to kick the can down the road by extending pandemic-era telehealth provisions (e.g., audio-only, in-home telehealth coverage) for an additional five months.
Did the COVID-19 pandemic accelerate the adoption of telehealth? Yes, but that growth is largely attributable to the law of small numbers, and utilization has already begun to taper. Did more individuals experience telehealth? Yes, but did telehealth reach the individuals it was intended to expand access for? Mostly not yet.
Two years into the pandemic, policymakers at all levels of government still lack a clear picture of who utilizes telehealth, where utilization is concentrated, and how individuals prefer to access healthcare services.
As a health economist and health-services researcher, I wondered who were the primary users of telehealth over the past couple of years: Has it actually expanded access to care, as it was intended and suggested by some of the prevailing industry narratives and recent surveys? The truth is, national utilization trends suggest telehealth appears to have not expanded broader healthcare access, with only a small number of people, in a certain segment, making up the majority of users.
Only 25.6% of Americans utilized a telehealth modality under the broadest definition of the concept. In contrast, almost 75% of Americans have not used telehealth during the pandemic. Telehealth accounted for nearly 30% of total digital health-funding dollars raised in the first half of 2021, but the impact of those dollars remains to be seen. Moreover, utilization data shows that telehealth is acting more like a luxury good.
During the pandemic, as many industries were forced to pivot to virtual operating environments, consumers had their choices restricted. The uptick in telehealth utilization is an example of how healthcare adapted to such restrictions—where doctors and patients relied heavily on virtual-care channels in the absence of an in-person healthcare experience.
But that shift hasn’t stuck. So to understand just how big the telehealth market is today—and who is actually using it—my colleagues and I dug into it and found that the total addressable market (TAM) is perhaps a lot smaller than many may think.
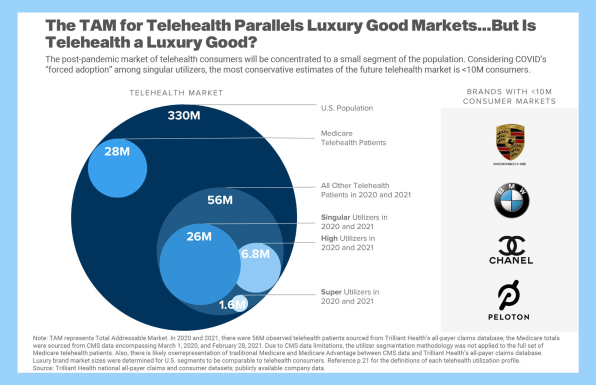
[Image: courtesy of Trilliant Health]
Our data show that the TAM for telehealth is less than 1% of the health economy, or approximately 10 million people out of the nation’s population of 330 million, where the vast majority of people would opt for in-person care if given the choice.
From a TAM perspective, telehealth’s U.S. market size of 10 million people actually mirrors that of luxury goods like Porsche and Chanel, which cater to specific segments of the population. Additionally, quarterly Peloton-connected workouts actually mirrored telehealth utilization, in markets of comparable size.
However, even with the fact that telehealth’s TAM represents only 10 million people right now, the reality for healthcare stakeholders (especially investors) is much more concerning. Within that population of 10 million, only a small subset of women drive telehealth’s demand today, and an increasing supply means there is simply not enough demand to go around.
Our analysis of claims data uncovered that the largest cohort of telehealth users is women, ages 21 to 40, who are commercially insured and are from more affluent geographies.
While demographics (e.g. age, gender, income) and utilization history can be useful dimensions for understanding what healthcare consumers do, they do not explain why consumers make the decisions they do.
That’s where psychographics are particularly useful. The use of psychographic segmentation—classifying consumers based on how they think, feel, and act—has historically been very useful across healthcare broadly. For example, the influx of information that consumers are receiving and perceiving about COVID-19 differs across the five primary psychographic profiles. Consumers in different psychographic profiles also tend to have distinct perceptions of care quality, which can influence their choices (e.g., why and when they may want to see their doctor via telehealth, in-person, or via a hybrid model).
The point is that consumers are complex individuals, but the market has not treated them as such. Headlines have suggested that telehealth’s appeal is much greater than reality. Add on top of that the misalignment of policies, still-evolving payment structure, wide-ranging consumer preferences, and health literacy challenges in certain populations, and our healthcare system has a long way to go before the full potential of telehealth can be realized.
Despite the fact that telehealth has been around for 20 years, and even with the incredible amount of investment funneling into the market, telehealth has yet to benefit the entire population, especially those who need more care—the most likely underserved and at-risk communities. While intended to be a tool that expands access to care, telehealth has only managed to give those with plenty of care even greater access.
The system, as designed, is not reaching telehealth’s targeted population—those who most needed expanded healthcare access. While factors, such as broadband (which has been a focus of existing policy efforts), influence, to some extent, teleheath adoption, the data suggest there are more variables underlying patient use (e.g., psychographics, demographics, clinical cases).
By first understanding the many reasons these consumers are not using telehealth more—including their ability to use it, awareness, physician incentives, individual preferences, price, broadband connectivity, or other—we will be better positioned to identify solutions to help telehealth reach its full potential as an access-expanding tool across income brackets. For now, however, what we do know is that the extension of telehealth provisions, while it has had some impact, doesn’t necessarily translate to more usage for the underserved.
Sanjula Jain, PhD, is the chief research officer and SVP of market strategy at Trilliant Health, and a professor at Johns Hopkins University.
(33)