How 3D printing could help save lives in war-torn Syria
For thousands of Syrian refugees who have suffered horrific blast injuries after being hit by barrel bombs and other devices of death in their war-torn homeland, the only option is amputation. When you see the damage a blast injury can do, it’s a shock to the system and is so very sad and upsetting.
Barrel bombs have been dropped throughout the long conflict that has torn Syria apart and caused untold misery and pain to so many innocent civilians. At the start of 2018, Amnesty International reported that barrel bombs had killed more than 11,000 civilians in Syria since 2012, injuring many more.
The barrel bomb is a type of improvised explosive device which—according to the UN—is used extensively by the Syrian Air Force. They are made from large oil barrels and are typically filled with TNT, oil, and even chunks of steel. Due to the large amount of explosives that can be packed into a barrel, the resulting explosion can be devastating.
Even if a person survives such a blast, their limbs are at risk of suffering a large, often jagged break, which, even in the best conditions, would be a major challenge to repair. In a fully equipped, state-of-the-art hospital, such patients would be able to access expert orthopaedic surgery and a lot of expensive aftercare.
But in a refugee camp, far away from any sophisticated surgical intervention, these types of complex procedures with timely recovery and care implications are just not possible. So at the moment, amputation is unfortunately the most likely outcome in many of these cases.
Many of these bone-shattering injuries are untreatable because of the constant risk of infection from procedures carried out in the field and the collapse of the healthcare system. A simpler and cheaper way to help these people needed to be invented, and my colleagues and I believe we have done just that.

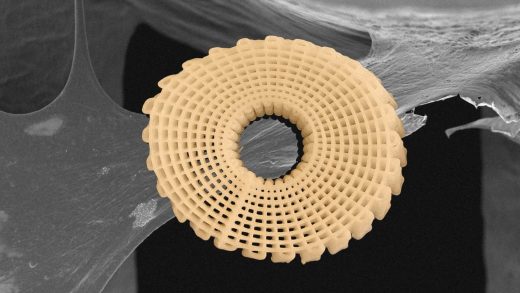
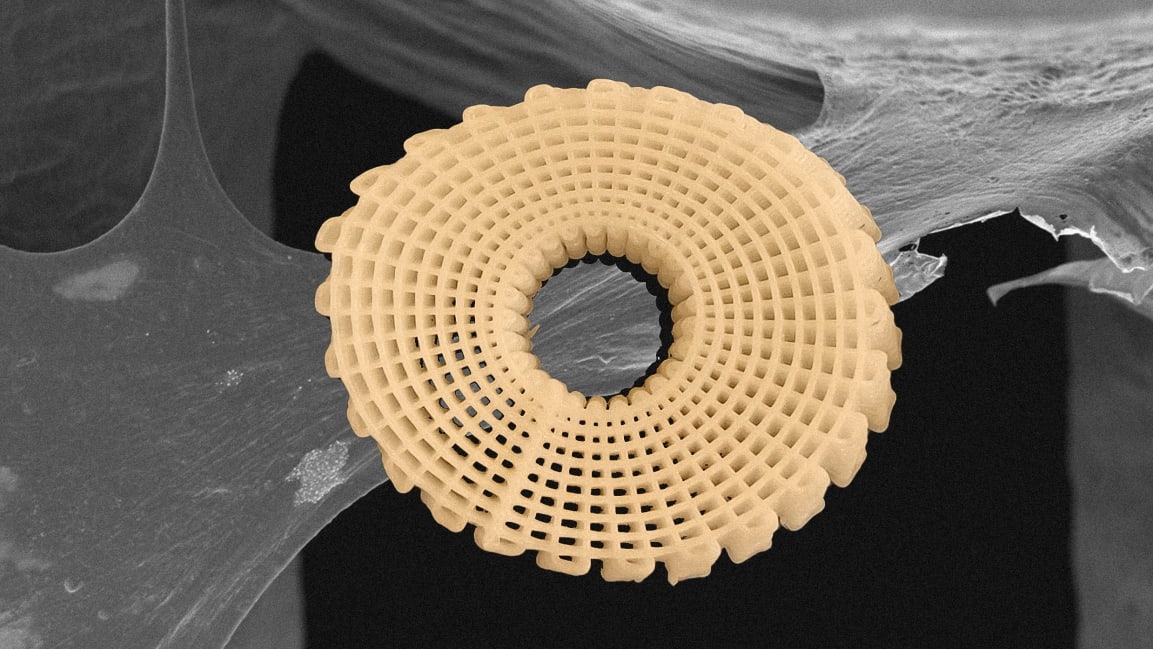
Our treatment uses a temporary, 3D-printed “bone brick” to fill the gap. They are made up of polymer and ceramic materials and can be clicked together just like a Lego brick to fit perfectly into whatever gap has been created by the blast injury. The bricks are degradable and allow new tissue to grow around them. This structure will support the load like a normal bone, induce the formation of new bone and, during this process, the bricks will dissolve. The idea is that the surgeon can open a bag of bricks and piece them together to fit that particular defect and promote the bone growth.
The solution has been a long time coming, and it was very much the plight of Syrian refugees that inspired it. It struck a very personal chord. I recognize that misery and pain and see my younger self on the faces of the children. I was born and grew up in Mozambique in Southeast Africa in 1968. It was the middle of the war of independence and the country was in turmoil.
My family inevitably became caught up in the decade-long conflict that involved the Portuguese community that was living and working in Mozambique and the Frelimo (the Mozambique Liberation Front) resistance movement that were seeking independence and self-rule.

[Photo: courtesy of the author]
It was 1973 and these were dangerous times. I was about five years old and it was a very frightening and disruptive period of my life. We moved up and down the country as my father’s job in civil administration changed and required us to move to the Niassa government base in Vila Cabral (now Lichinga).
One episode sticks out vividly. My 1-year-old brother, Jose Manuel, and I were taken from our home in Maragra and moved to a refugee camp in an area of South Africa called Nelspruit, as we tried to escape the escalating violence. We were safe but I was always anxious and scared about the security of our family.
Although we were only in the camp for around a month before we were transferred to start a new life in Portugal when I was 6, that experience stayed with me for life. It gave me a strong sense of empathy for others who are being displaced by war. And it would eventually strengthen my commitment to use my bio-medical expertise to try and do something to help other refugees.
Blast injuries and amputations
The first time I was made fully aware of the impact of blast injuries in the Syrian conflict was when Amer Shoaib—a consultant orthopaedic surgeon at Manchester Royal infirmary—came to my university to discuss his experience and the problems he faced in treating these injuries in Syrian refugees.
Shoaib is a limb-injury expert with experience of working on the frontline of various conflicts and crisis zones as a humanitarian worker. He told us that in Syria the aftereffects of blast injuries were sometimes untreatable because of the constant risk of infection. The collapse of the healthcare system has also led to many treatments being done by people who are not, in fact, trained medics.
Shoaib was working in refugee camps in Turkey and I, along with my Manchester research colleagues Andy Weightman and Glenn Cooper, decided we needed to help and apply our expertise. We all wanted to make a difference and we continued our discussion late into the evening. This conversation developed into the idea of the “bone bricks.”
A game-changer
My own academic interests include biofabrication for tissue engineering. This involves fabricating bone, nerve, cartilage, and skin through the use of 3D printing. 3D-printing technology can now reproduce biocompatible and biodegradable materials that can be used in the human body.
Current grafting techniques have several limitations, including the risk of infection and disease transmission. They are also quite costly and present a high risk of further injury and serious bleeding. This work is centered on creating orthopaedic devices—or scaffolds—that can enable the regeneration of bone tissues to repair fractures.
I had been busy responding to the calls from clinicians to make these tools more agile, smaller in scale, and responsive to more personalized healthcare. But the challenge set by the Syrian situation was a game-changer: We had to consider other new factors, such as making the scaffolds even more cost-effective and useable in demanding environments where it is very difficult to manage infection.
Part of our solution to these challenges was to use relatively low-cost 3D-printing technology to create bone bricks with a degradable porous structure into which a special infection-fighting paste can be injected. The bone brick prosthesis and paste will prevent infection, promote bone regeneration, and create a mechanically stable bone union during the healing period.
The challenge of creating this pioneering prosthesis led us on a journey to Turkey in 2016 where we met with academics, surgeons, and medical companies. We were convinced that our proposed new technique could dramatically improve the medical response to life-changing limb injuries in the challenging conditions of these camps. It was clear that our project should be focused on patients within the Syrian refugee community in Turkey where they have found a safe haven from the horrors of war.
Once we secured the backing of the Global Challenges Research Fund (a $1.86 billion pot provided by the U.K. government to support cutting-edge research that specifically addresses the challenges faced by developing countries), we began to put our project into motion. As a first step Weightman, Cooper and I visited Sabanci University in Istanbul to meet with our lead collaborator there, Bahattin Koç, who introduced us to a group of clinicians who had been dealing with the refugees and their injuries firsthand and were able to share their knowledge. Their experiences gave us insight into the challenges of treating serious bone injuries in the field.
Our collaborators in Turkey helped ensure we shaped the design and specifications of the bone bricks so they aligned as closely as possible to the needs of the front-line clinicians. During our stay in Istanbul we were constantly reminded of the human cost of the Syrian civil war. We would often witness groups of displaced families, including children, who had fled the conflict and were seeking refuge and the chance to rebuild their lives. What we had seen on TV about Syria, with helicopters dropping bombs, was brought home to us. Some of my colleagues have children the same age as those we want to help, and it made us even more determined to do something.
War in Syria
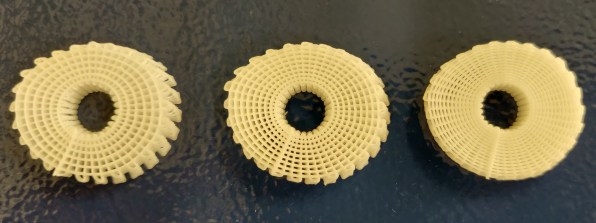
The Syrian conflict has displaced around 3 million refugees into Turkey, accounting for around 4% of its population. Turkey provides free healthcare services to Syrians and, as such, the burden on the healthcare system is significant, with 940,000 patients treated, 780,000 operations, and 20.2 million outpatient services taken up between 2011 and 2017 alone.
The Turkish government says it has spent more than $37 billion hosting Syrian refugees. We hope that our bone bricks innovation can make a contribution to this crisis, helping to mitigate Turkey’s healthcare costs and also significantly improve the human cost of this crisis.
Our project is focused on bone injuries that are often caused by blast explosions, which are powerful enough to throw a person many yards and shatter bodies. Shoaib once said to us:
This is certainly true for the Syrian crisis where thousands of people are suffering terrible injuries. Given that almost 2 million people have been injured in the Syrian civil war, we estimate that 100,000 people have been affected by large bone loss, and of those injured since 2013 there have been more than 30,000 amputations—equating to about 7,500 a year. Amputation has associated physical complications including heart attack, slow wound healing, and the constant risk of infection.
Catastrophic limb amputation
Current bone repair techniques are complex. They include:
And it must be remembered, traumatic limb amputation is a catastrophic injury and an irreversible act that has a sudden and emotionally devastating impact on the patient. As a consequence, this not only impacts a person’s ability to earn a living but also brings very serious psychological issues for the patient because of the cultural stigma associated with limb loss.
External prosthetic limbs after amputation provide some with a solution, but they are not suitable for all. Studies show that the long-term healthcare costs of amputation are three times higher than those treated by limb salvage. Clearly, saving a limb offers a better quality of life and functional capacity than amputation and external prosthetics.
Just like Lego
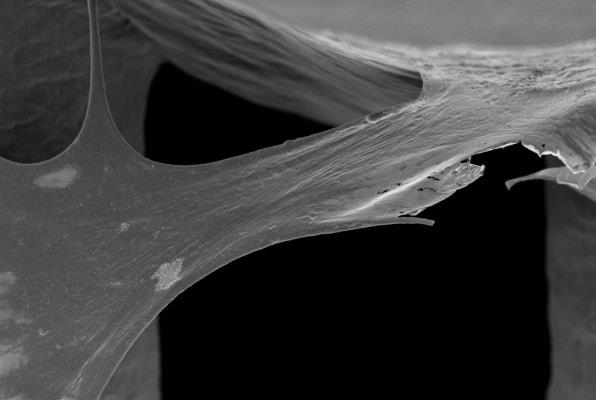
With many blast injuries, the bone defects are totally impossible to heal. What we are doing is creating a temporary structure using bone bricks to fill the gap. Our treatment uses medical scaffolds, made up of polymer and ceramic materials, which can be clicked together like a Lego brick, creating a degradable structure which then allows new tissue to grow.
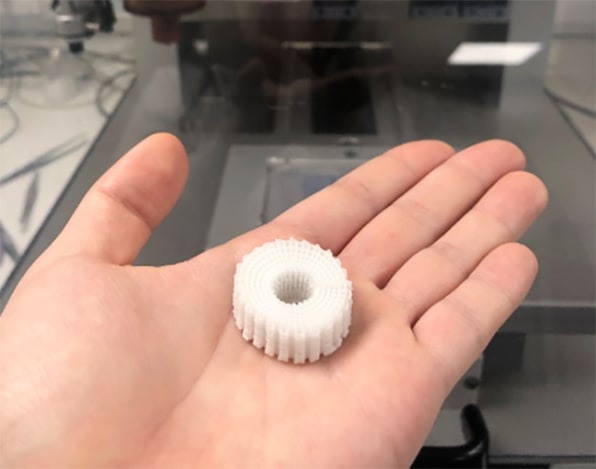
[Photo: courtesy of the author]
We are also developing software to allow the clinician, based on the information on the bone defect, to select the exact number of bone bricks with the specific shape and size and information on how to assemble—just like Lego instructions. The connection between the bone brick design and the 3D-printing system is completed. We’re now in the process of integrating with the software that will link the scanning of information from the wound area with the identification of the correct type of bone bricks and assembly mechanism.
An antibiotic ceramic paste is stored in a hollow in the middle of the brick and is a highly practical way to combat infection while the limb repairs and hugely improves the chances of success.
The bone brick solution is much more cost effective than current methods of treatment. We expect our limb-saving solution will be less than $250 for a typical 100mm fracture injury. This is far cheaper than current solutions, which can cost between $335 and $1,250 for an artificial limb depending on the type needed.
When will they be used on humans?
My team and I are entering the final stages of a three-year project. Our team consists of academics and clinicians from Manchester and Turkey, as well as a pool of ten bone injury patients drawn from the U.K., Turkey, and Syria. We have already evaluated the modular bone bricks system in a computer simulation, created prototypes of the modular bone bricks using 3D-printing technologies in the lab, and conducted in-vitro (laboratory) testing of mechanical and biological characterization of the bricks. This will be followed by in-vivo (animal) testing to prepare the device for regulatory approval and a pathway to implementation by clinicians. Once all these stages are complete the project, we will be ready to trial on human patients.
The final stage will then be to translate the research into building a useable, medical device. This will be undertaken by a follow-on clinical trial on about 20 patients with large bone loss, some of which we expect will be drawn from the Syrian refugee community. The project will be subject to strict ethical scrutiny and approval.
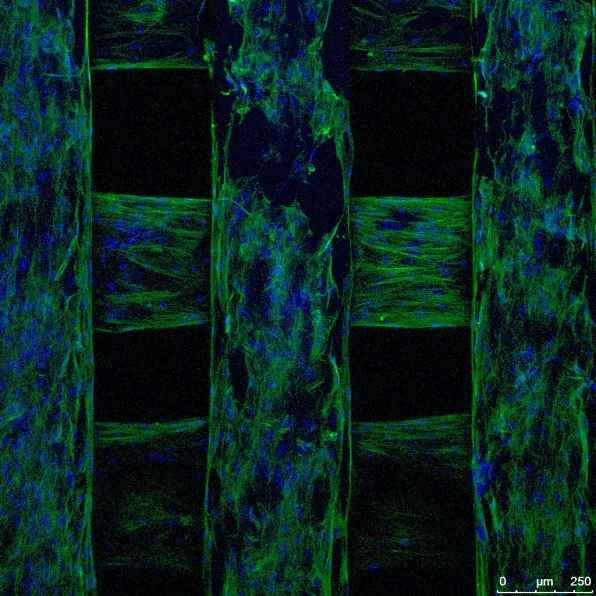
[Image: courtesy of the author]
We hope this project will lead to further development of emergency healthcare in the developing world and could bring hope to a Syrian refugee community in dire need while their country rebuilds. Our long-term hope is that bone bricks will be of use, not only in refugee crises, but also in many other healthcare situations, such as accidents and natural disasters—in both developing and developed nations. For example, in the U.K. around 2,000 patients a year receive treatment for severe fractures requiring surgical reconstruction for bone loss.
The burden to the health service relating to major traumatic injuries is estimated to be in excess of $0.6 billion. In addition, the estimated loss of contribution to the economy due to extended periods of rehabilitation is another $4.3 billion.
We believe the bone brick project could help alleviate some of those economic burdens and drastically improve the patient experience. But it is the plight of the Syrian refugees that continues to inspire and inform this project. We hope that, perhaps in five years’ time, bone bricks will be used in the field on humans, finally giving medics and victims an alternative to catastrophic limb amputation.
Paulo Bartolo is chair professor on advanced manufacturing at the University of Manchester. This article is republished from The Conversation under a Creative Commons license. Read the original article.
(71)