On a recent day in January, a drone took off from one corner of a remote island in Vanuatu and delivered vaccines to a health clinic in another part of the island–a journey that would normally require hiking through miles of rough, muddy trails or an expensive boat ride. It was the second month of testing for a system that could help vaccinate thousands of children living in the hardest-to-reach parts of the Pacific archipelago.

Vanuatu, which sits hundreds of miles west of Fiji in the Pacific, is made up of around 80 mountainous islands separated by hundreds of miles of often-rough seas, with few places to land a boat. On any given island, it’s hard to travel between communities. “If you need to get a vaccine to rural health centers, there are few opportunities,” says Shelton Yett, the Pacific representative for UNICEF, which partnered with the government in Vanuatu to test the drones. “Nurses can slog through the mud with a vaccine carrier on the shoulders. In high heat, they don’t go. If it’s raining, as it is now, you can go a long time without restocking health clinics. So we’re always looking at new ways to improve the supply chain, and new ways to get vaccines to the children who need them most.”
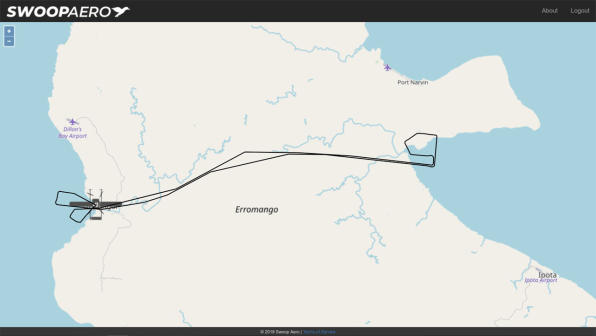
[Image: Swoop Aero/courtesy UNICEF]
The government has made progress in improving vaccination rates, but around 20% of children weren’t getting vaccinated against life-threatening diseases; UNICEF had experimented with drone delivery in other countries and thought that it could help. Swoop Aero, the first drone company to participate, started making its first flights in December. The drones, with an 8-foot wingspan, can fly in rain and gusts–although not the cyclone that the country is currently experiencing. A drone can carry five pounds of vaccines, ice packs, and a monitor that ensures that the vaccine stays in the narrow temperature range necessary for it to work.

The company only gets paid if the vaccines are delivered successfully. “It’s the first commercially sustainable system,” says Yett. “You can have all sorts of wonderful things if you keep throwing money at a problem, but of course there’s not enough money to go around in the development business, and that’s why we need to make sure it’s [financially] sustainable.”
In the trials, the government is testing whether the drones can dependably deliver vaccines when health centers make a request; whether the vaccines arrive safely; whether the drones interfere with aviation; and that communities don’t panic when they hear the loud, unfamiliar buzz of the machines. (Before the program began, communities were invited to test flights to learn about the technology, when the first official flight happened.) To date, around 40 children have been vaccinated.

In a couple of weeks, the first trial will end, and the government will decide if it wants to go to the next stage, which will involve training local drone operators. The drones could also eventually be partially 3D-printed in Vanuatu. The technology, Yett says, isn’t a complete answer. “It’s very easy to be distracted by bling,” he says. It’s still necessary to educate parents about why vaccination matters–and why it’s important to come to clinics on a set schedule–and to train nurses and maintain the supply chain. But the drones are a promising solution for one piece of the problem.
Others are beginning to do the same thing elsewhere. Zipline, a startup that began using drones to deliver blood for transfusions in Rwanda in 2016, recently began to test vaccine deliveries and will launch a regular service in the next few weeks. It also plans to begin delivering vaccines, along with other medical supplies, when it starts operating in Ghana this spring. Drone deliveries of vaccines could also begin to happen in other remote regions. “If this can work in Vanuatu, it can work anywhere,” says Yett.
(29)