The healthiest communities in the U.S. are the ones where people can afford homes
North St. Louis County, Missouri, faces numerous challenges: The unemployment rate is three times higher than in the rest of the U.S., and life expectancy is 15 years lower than in Clayton, a more affluent community just three miles away. Over 90% of schoolchildren qualify for free school lunches, and all get their education from a system that lost its state accreditation six years ago. On top of that, North St. Louis County presents an organizational quandary: It comprises 24 distinct municipalities–some, like Glen Echo Park, as small as 150 people–each with their own separate government. When you think of the difficulty of coordinating resources across a single city, consider the challenge of trying to serve 36,250 residents of an 11-square-mile region through 24 administrative channels.
During the foreclosure crisis of 2008, when thousands of families across North St. Louis County defaulted on their mortgages, housing instability constricted families’ ability to access food and other necessities. Unable to meaningfully address the crisis afflicting the whole county with such a disjointed governance model, leaders in the 24 municipalities decided to override it and unify. The resulting alliance, 24:1, has built out a community garden and more youth programming to supplement the schools, which were reaccredited in 2017. And to begin to remedy the issue that sparked the initiative in the first place, 24:1, with the local nonprofit Beyond Housing, has set up a community land trust–a nonprofit-managed, permanently affordable housing development–to rebuild homeownership opportunities in North St. Louis County.
For that work, 24:1 was named a Culture of Health Prize winner in 2016 by the Robert Wood Johnson Foundation (RWJF), which funds initiatives that boost the overall health of communities. Every year, RWJF announces a set of Culture of Health awardees, and also releases, in partnership with the University of Wisconsin, a ranking of the overall health of every county in the U.S. (you can access the interactive rankings here). The County Health Rankings, which were first developed by researchers at the University of Wisconsin as a way to compare different counties and outcomes for their residents across the state, analyze a variety of factors to determine overall county health. Traditional health metrics like obesity and smoking rates factor in alongside broader indicators like access to education, public transit, and air quality.
The County Health Rankings are designed as a tool to compare county health within states, not across state lines. (RWJF points to America’s Health Rankings for state-by-state comparisons.) Focusing on in-state comparisons, RWJF hopes, will keep the focus on solutions similarly local: When looking at how to address the needs of a struggling county in Louisiana (which consistently falls at the lower end of the Health Rankings spectrum) like East Carroll, for instance, it’s more meaningful to look to more prosperous counties in the state, like St. Tammany, than to try to source pointers from Kauai, Hawaii–the healthiest county in the United States in 2018.
This year, RWJF and the University of Wisconsin decided to focus on an issue that unites nearly all counties in the U.S.: access to good and affordable housing. “Housing impacts health in so many ways,” says RWJF program officer Abbey Cofsky. Through the report, they wanted to draw attention to its role, and ways that communities and other organizations can center on housing needs in the conversation around health. North St. Louis County features prominently in the report–this time as a model the report authors hope other communities struggling with housing issues can learn from.
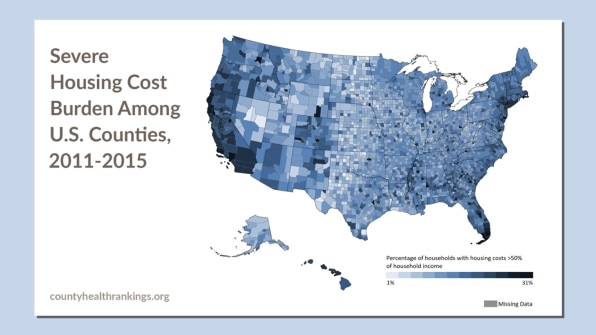
There’s no question that across the U.S., access to housing is a persistent issue. Over 1 in 10 households in the country are overburdened with housing costs that take up more than half of their income. That leaves little left over, Cosky says, for families to afford food and necessities like medicine, which has implications for health. These housing-related challenges are present in communities across the U.S., but are especially pronounced in more segregated places (the 24:1 community, for instance, is more than 80% black).
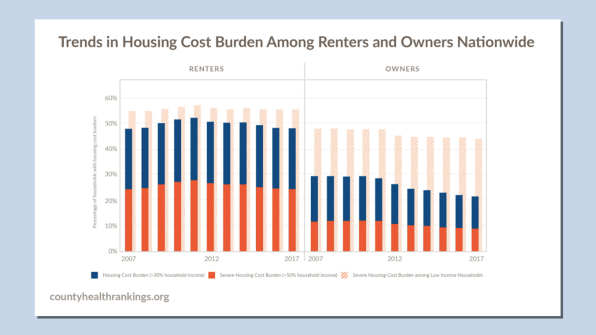
While the number of households severely cost-burdened by housing has declined in large metro areas since the recession, it’s grown more pronounced in the rest of the country. Renters, more than homeowners, are affected (as shown in the data above), which is why initiatives like the 24:1 land trust that emphasize affordable homeownership are crucial.
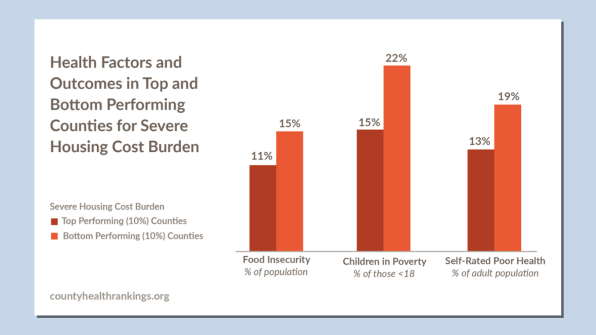
The 2019 County Health Rankings show a clear correlation between prevalence of housing cost burdens and negative health outcomes. The counties where the highest percentage of households struggle with housing costs also show elevated rates of child poverty, food insecurity, and poor overall health among adults. Bronx County, New York, is the most housing-cost-burdened county in the U.S.: Around 32% of residents devote over 50% of their income to rent, and nearly one-third report poor overall health. Food insecurity rates hover around 16%, and nearly 40% of children live in poverty. The Bronx struggles with housing, in part, because of its proximity to Manhattan, one of the top three most expensive real estate markets in the U.S. (Like San Francisco, Manhattan’s housing cost burden is high, but not extreme, because of the disproportionate number of very high-income people who live there and who do not experience a cost burden, despite how much they pay for a home.)
But high housing costs are a factor across urban, suburban, and rural parts of the U.S. In southern Illinois, for instance, around 20% of Jackson County’s residents are extremely housing-cost burdened, and that issue tracks with other difficulties: Over 30% of children live in poverty, and 16% of adults report poor health.
RWJF found that across counties in the U.S., every 10% increase in the share of households severely cost-burdened by housing equates to 29,000 more children in poverty, 86,000 more food-insecure people, and 84,000 more people in poor health.
RWJF and the University of Wisconsin want the rankings to serve as a reminder of what really constitutes health. Everything from the history of segregation in the U.S. to availability of good food in communities plays a role. But a good, affordable place to live is the grounding force. For 24:1, the focus on stabilizing housing for families has enabled community members to become more involved in local initiatives like community gardening, and has freed up financial resources for them to access care at a new clinic. Since the initiative launched, both infant mortality and youth obesity have significantly declined in the community.
Counties that see in the rankings that housing costs are a burden on residents should pursue initiatives like the 24:1 community to stabilize households in place and free up resources for other key contributors to health, like green space and fresh food. But Cofsky also points to how healthcare practitioners can take a more active role in ensuring housing needs are met. The fact that Kaiser Permanente is funding affordable housing in Oakland, she says, is a sign that the link between housing and health is becoming clearer, and might drive other such investments across the country.
(11)



