In the 1850s, London’s Soho neighborhood was a thick layer cake of tenements separated only by narrow footpaths, a prime breeding ground, it turned out, for the 1854 cholera outbreak. One young London doctor, John Snow, sought a scientific explanation for rampant disease in the newly minted capital of industrial wealth.
Instead of emptying the city, as had been done in prior outbreaks, he placed a mark on a map of Soho where each cholera case had emerged. At the largest cluster of markings—a clear nucleus—Snow isolated a water pump where a broken sewer pipe was dumping human waste into the drinking water. He had the handle of the pump removed, and the outbreak in the area declined. Snow’s research proved that cholera was not morally borne; it was waterborne. The roads and alleyways, the buildings built among them, and the pipes laid beneath them—mixing and pooling human waste— enabled the disease to spread. He also proved that biological survival is spatially reliant.
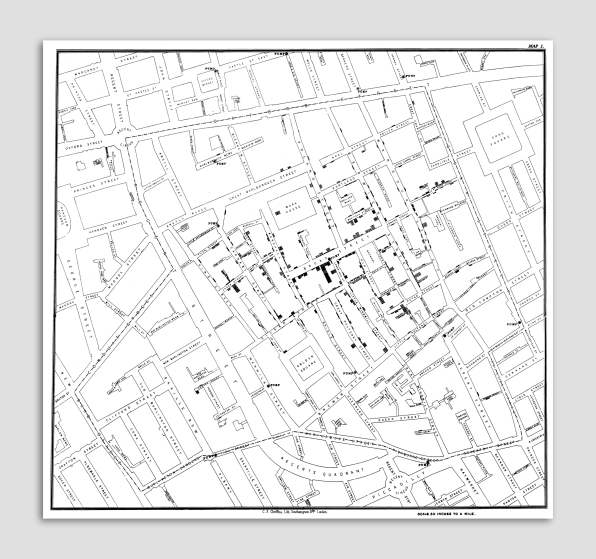
[Image: Wiki Commons]
Snow’s simple mapping method is a foundational document in the study of disease and of the design of cities. Cited as a founding father of epidemiology and urban design alike, he demonstrated that poor (or nonexistent) spatial planning puts public health at grave risk. He also revealed a structural solution that was (at least empirically) blind to class, linking the working-class neighborhood of Soho and the workers’ health to the health of the public at large.
A redesign of piped city substructure, increased zoning and regulatory superstructure, and the decongestion of dense tenement housing in industrial capitals such as London and New York followed in the latter part of the 19th century—all under the rubric of health, sanitation, and hygiene.
[Photo: Robert Howlett/Metropolitan Museum of Art/Wiki Commons]
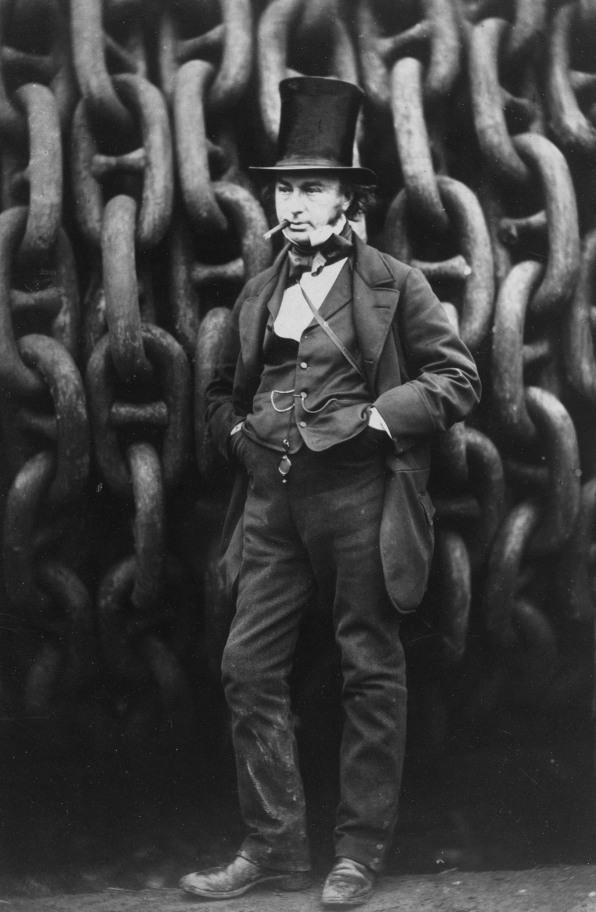
These new theories of contagion were circulating among health care professionals in the 1850s, when Isambard Kingdom Brunel, one of England’s most famous engineers, was tasked with designing a demountable military clinic for Crimea. His design accordingly homed in on the essentials: controlled access to light and fresh air, the separation and removal of waste, and the prevention of overcrowding. Snow’s discovery contributed to a growing body of evidence that challenged miasma theory, but the latter would continue to dominate medical planning for another half-century.
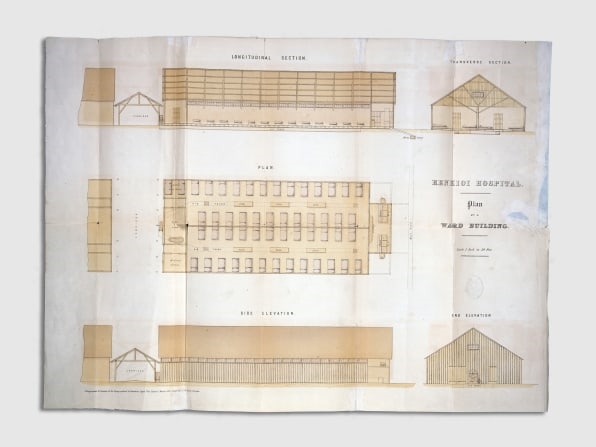
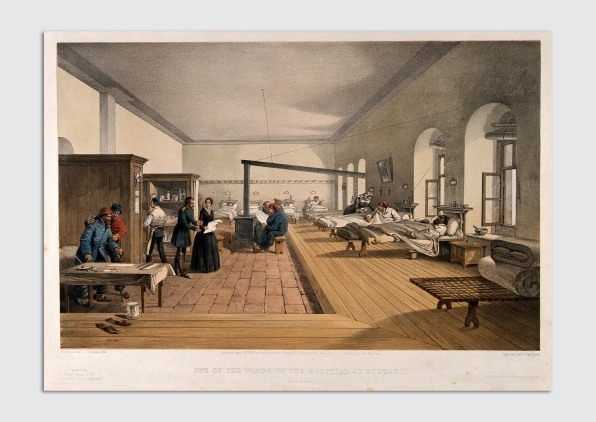
[Image: Wellcome Collection/Wiki Commons]
Brunel delivered a never-before-seen structure: a flat-packed, prefabricated emergency field hospital. His replicable unit—a single ward—was lightweight, made of wood, and covered in a thin layer of tin that acted as insulation. It was extremely well ventilated, with a series of openings running under the eaves, two long rows of narrow windows designed to let in air even when shuttered, and a rotary air pump at one end of the structure for hand-crank ventilation when needed. Each ward was designed to be self-sufficient, containing its own lavatory, nurses’ room, storage facility, and surgical theater. Before the hospital was deployed to Turkey, a prototype was erected in Paddington station.
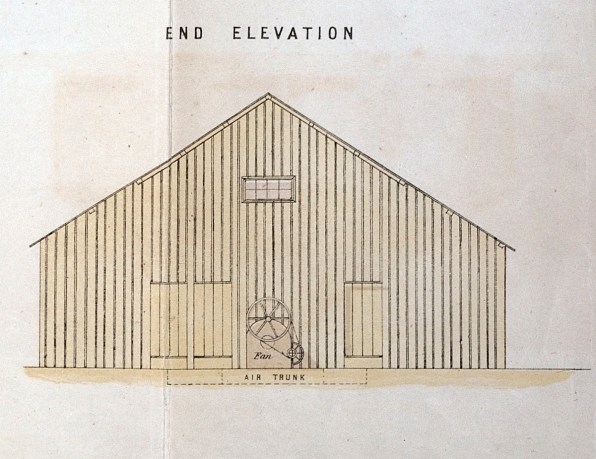
[Image: Wellcome Collection/Wiki Commons]
Construction of Brunel’s field hospital began on May 21, 1855, in the Turkish town of Renkioi. Less than two months later, on July 12, it was ready to treat 300 soldiers. By August 11 it housed 500 patients; by December 4, 1,000, and by the end of March 1856, when the war ended (less than a year after construction started), the hospital had expanded its capacity to 2,200 beds. Prefabricated and incremental construction meant that the hospital could be rescaled as demand waxed and waned.
The industrialization of England influenced warfare and occupation abroad. The prefabrication of prototypes is an industrialized building method; scale, replicability, and speed are the priorities, not craftsmanship. For Brunel’s design, context, culture, and site mattered little: the goal was a temporary structure that could be erected quickly and function more effectively. And in Renkioi, the goal of treatment was not a reduction in suffering so much as the protection of military assets, the prolonging of British soldiers’ lives so that they might more decisively shorten the lives of the enemy. In this way, health care was also industrialized.
By the end of the war, the mortality rate at the Renkioi hospital was around 3%; in Scutari, a nearby barracks hospital where Florence Nightingale worked, the mortality rate was 42.7%.This 40% difference was evidence of the profound impact of simple architectural and spatial methods—methods that, when fully understood and replicated, would go on to prolong untold nonmilitary lives. The hospital, no longer a hall of the dead, was now a mechanism of science and its architecture a humanitarian conduit to a longer life.
The Nightingale Era
The Renkioi hospital’s enduring influence is due not to Brunel but to Nightingale, who had an opportunity to observe it while nursing in nearby Scutari. In her book Notes on Hospitals, she described the components of the pavilion hospital and praised its logic and scientific rigor. The ideas Nightingale set forth are generally considered the first treatise on modern hospital planning and quickly became foundational references for hospital design. Nightingale presented an extensive list of standards: for example, wards should be no more than two stories high, beds should be at least three and a half feet apart, and all woodwork should be finished in such a way as to allow for quick washing and drying. In all her writings, she stressed the importance of clean air above all: “The very first canon of nursing…is this: to keep the air [the patient] breathes as pure as the external air, without chilling him.”
[Image: Wiki Commons]
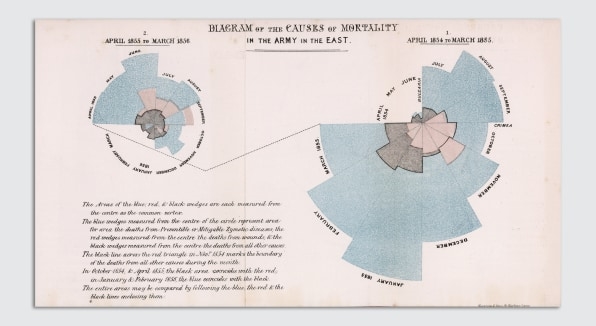
Nightingale’s various publications contained detailed records and pioneering visual graphics. The rose chart, or coxcomb diagram, is attributed to Nightingale, who used it to quantify and compare the prevalence of preventable wartime deaths. Notes on Hospitals also contained architectural drawings, which described the benefits, dimensions, and parameters of the ideal hospital ward.
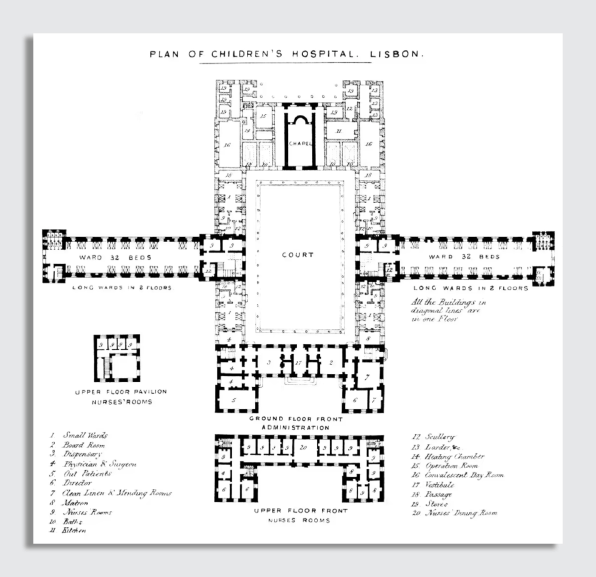
[Image: Wellcome Collection]
By the late 1800s, Nightingale’s design—the pavilion ward—was deployed around the world, another colonial beachhead in the sanitation era. This standardized, replicable model (known also as the Nightingale ward) transformed hospitals from buildings full of beds into vital instruments of health.
In the spring of 2020, the COVID-19 pandemic stretched hospitals around the world beyond capacity. The infection of doctors and nursing staff showed early on that the virus was airborne, and the movement of air, that age-old hospital problem, became a dominant criterion in the prevention of contamination. As in the Crimean War field hospital in Renkioi, 170 years ago, it became essential to ensure the separation of beds, to provide protected observation points for nurses, to prevent the contamination of equipment, and to isolate patients. And as was true in Crimea and during the influenza pandemic of 1918, the window and the flow of air received the most attention.
Medical professionals at Mount Sinai Hospital in New York moved COVID patients from modern air-sealed buildings to a 1930s bed tower that had windows designed to be opened, retrofitting those spaces with in-room filters and fans. Suddenly, the hospital’s reliance on machine air-conditioning was a weakness, a reminder to planners that certain universal, spatial principles—notably that buildings must provide access to uncontaminated air—should not be designed around. The machine, in this way, had broken a primary law.
Like all crises that reveal cracks in the system, the pandemic has prompted a public reckoning with the role of buildings in shaping our health. Recent reporting is waking up to the crisis of breathability in buildings, raising questions about our dependence on mechanical systems and the lack of access to fresh, natural air. Why are so many buildings filled with inoperable windows? How did we not foresee the dangers of creating an airtight seal around entire city blocks? Is it really acceptable that our built surroundings are entirely dependent on evermore complex mechanical systems that pollute the environment and, if they should fail, prevent us from breathing?
At our peril, we have ignored Nightingale’s prescriptions. The history of the hospital contains clear lessons about the importance of air movement through buildings, the public health risks of poor design, and the dangers of technological reliance. Architecture professionals should look back to see what else has been forgotten or ignored in the race to merge art and technology. Whose lives might be at stake if they don’t?
Excerpted and adapted from The Architecture of Health: Hospital Design and the Construction of Dignity, an accompanying publication for the Design and Healing: Creative Responses to Epidemics exhibition, on view at Cooper Hewitt, Smithsonian Design Museum through February 2023
Michael Murphy, Int FRIBA, is a founding principal and executive director of MASS Design Group, a collective of architecture and design advocates dedicated to the construction of dignity. MASS is the recipient of the 2022 AIA Architecture Firm Award.
(49)