The Rise Of “Biorights”: Patients Demand Cash, Control For Donating DNA
Mary O’Connor had long wanted researchers to decipher her genetic code to better understand a deadly heart condition that runs in her family. But the 52-year-old woman balked at providing a saliva or blood sample to researchers because they would neither promise to give her the results nor pay her for her trouble.
O’Connor, of Nantucket, Massachusetts, finally submitted her sample in March after a start-up medical company, DNAsimple, gave her $50 for it—no windfall, but enough to meet the monthly co-payments for three of her medicines. Plus, she’ll get another payment every time a new sample is needed.
Human DNA derived from biological samples—a valuable research commodity in medical research—is in high demand as drug companies, the government and academic centers race to collect and analyze specimens. One research firm predicts that biological samples like those DNAsimple collect will generate $23 billion in revenue by 2018.
At the same time, rising public awareness of the value of genetic data and high drug costs are dramatically changing patients’ traditionally passive role in research. Before providing specimens, patients are increasingly looking for compensation, commitments that useful medical information will be returned to them, or control over how their biological samples will be studied.
“Innovation and progress will save lives eventually, but only if a patient has the financial means” to afford the new treatments, said O’Connor, who asked that her maiden name be used to preserve her privacy. “There has been an over assumption and a gross expectation of patient altruism.”
The potential for modern medical research to exploit patients was spotlighted in a 2010 bestseller, “The Immortal Life of Henrietta Lacks,” that documented how a poor black tobacco farmer’s cancerous cells outlived her, fueling major medical discoveries. The cells were taken during treatment without her consent or compensation, and were later commercialized.
Since then, patients looking for more control over their tissue and its genetic revelations have drawn powerful allies. In May, the American Civil Liberties Union filed a federal complaint on behalf of four people against Utah-based Myriad Genetics Laboratories Inc. The group asked the U.S. Department of Health and Human Services to ensure patients have access to all the genetic data a testing company gleans from their samples, not simply whether or not they have a certain gene or condition.
DNAsimple, launched less than a year ago, is one of the few companies to pay for routine biological samples such as saliva. The $50 O’Connor received is about what a donor usually gets for blood plasma.
DNAsimple has already signed up almost 4,000 people, including O’Connor, who are contacted when a company needs a sample. Patients “feel part of the process when they get compensated,” said Olivier Noel, the chief executive officer of DNAsimple.
In some ways, the emerging “biorights” movement is making researchers nervous.
Health and Human Services and 15 other federal entities have proposed a controversial new requirement for researchers to get patients’ permission to study biological material such as blood, pieces of tumors or other tissue left over from routine and surgical medical procedures, even if researchers don’t know the donor’s identity. Currently, consent isn’t required for such samples.
Tumor Shortage?
Leading academic organizations, including the Association of American Universities and the National Academies of Sciences, Engineering and Medicine, oppose the rule, saying too many restrictions and costs placed on tissue and DNA collection will slow down researchers and stifle medical advances. “We may not get enough samples” to study, said Dr. Alexander Lazar, a pathologist at the M.D. Anderson Cancer Center in Houston.
Lazar said he already has difficulty finding enough Desmoid tumors, rare fibrous masses that can strangle arteries and compress organs, to study. If the federal proposal goes forward, he worries that the community hospitals that supply him may not have the time or resources to solicit patients for consent, leaving him unable to retrieve tumors.
Yet, many patients say that researchers too often take their contributions for granted, taking their fluid and tissue samples for research and offering nothing in return. Not only should researchers be required to get permission to study their tissues, these patients say, they should give patients information from the research that may help them.
“If you study my DNA, just let me know what you find,” said Stacey Tinianov, of California, who was diagnosed with breast cancer three years ago, six weeks after her 40th birthday. “I don’t think that is too much to ask.” Tinianov is one of more than 2,000 parties who have sent comments on the rules to the FDA.
With the price of some new biotech drugs rising into the six figures some patients whose genetic samples may lead to the next expensive breakthrough want something in return, much the way subjects are compensated for time and travel for participating in clinical trials.
“There is an economy around this data,” said Sharon Terry, chief executive officer of the Genetic Alliance, a patient advocacy group based in Washington. “Why shouldn’t the consumer be part of it?”
In fact, poll results show that people are far less charitable about helping researchers when they know the researchers’ companies stand to make money from them.
About 68% of people are willing to give permission for their specimens to be used by a researcher for any purpose, according to a 2015 study in the Journal of the American Medical Association. But support dropped to 55 percent if patients knew their sample would be used to “develop patents and earn profits for commercial companies.”

Freezer Farms
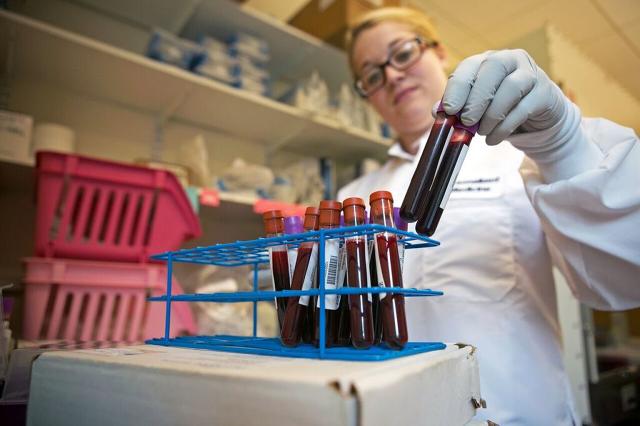
Troves of biologically valuable human samples are known as biobanks in the medical industry. Researchers familiar with one cache in Cambridge, Massachusetts, simply call it the “freezer farm.” It’s a half-empty room where Partners Healthcare medical system stores specimens derived from blood of more than 47,000 people in 16 large gray freezers at minus-80 degrees Celsius.
To stock it, Massachusetts General and Brigham and Women’s hospitals send emails and deploy recruiters to waiting rooms asking patients to donate three small tubes of blood to advance medical research. The blood is processed, yielding DNA information, serum and plasma, and frozen in vials marked with a unique barcode linked to patients’ de-identified medical records.
About 6,000 researchers affiliated with Partners can tap into the biobank for samples or data for about $20 a pop, to study how genes, environment and lifestyle affect people’s health. If a researcher collected a sample on his own, it would cost $400 or more, according to Scott T. Weiss, scientific director of Partners Healthcare
Personalized Medicine
Although data are hard to come by, one 2013 study found more than 600 biobanks in the U.S. alone, built by hospitals, industry and others.
Though patients don’t often share in the profits of biomedical research, they do sometimes get useful information, as in a partnership between New York-based Regeneron Pharmaceuticals Inc. and Geisinger Health System, with treats four million people, mostly in Pennsylvania.
Willing Geisinger patients provide Regeneron with DNA samples, and in return, if genetic sequencing reveals something considered “medically actionable”—such as discovering a woman has the BRCA gene that dramatically increases her risk for breast and ovarian cancer—Geisinger confirms the finding and then contacts the patient. So far about 140 of the more than 111,000 patients who have agreed to have their DNA studied have had results returned.
In Boston, the Partners group, which aims to get 100,000 volunteers, said it will start returning some medical information to patients this month.
Big drug companies are also in the market. Both Pfizer Inc. and the Genentech unit of Roche have bought access to genetic information from 23andMe, a California-based company that sells DNA analysis services to consumers. Genentech’s deal with 23andMe to study Parkinson’s disease was reportedly worth $60 million. The companies didn’t disclose terms of the deal.
People have long been paid for parts of themselves, notably in the reproductive field, where sperm can bring $600 a vial or eggs can fetch $10,000, according to fertility websites. Breast milk sells for $1 to $2 an ounce. But payments for donated biological samples for research have been rare. The U.S. Food and Drug Administration allows blood to be sold, but major collectors like the Red Cross have taken a stand against it out of fear that cash would incentivize donors to lie about contagious conditions and imperil transfusion recipients.
Nonetheless, the Red Cross website recently offered a $5 Amazon.com gift certificate for blood donors. Online, researchers can buy a breast tumor sample for $230 or more. A vial of blood cells often used by immunotherapy researchers can sell from $540-$820, according to a review of websites by The Eye. Researchers say prices, especially from patients with rare conditions, can increase by as much as fourfold when the sample is linked to a de-identified personal medical record that researchers can plumb to understand where genetics, environment and lifestyle intersect.
Ken Deutsch, a bladder cancer survivor in Cambridge, Massachusetts, was tested by Myriad Genetics in 2014 to see if he had a genetic mutation that could make him more responsive to a certain treatment. Myriad told him he had the mutation, but Deutsch wanted more detailed information so he could share it in a public database that researchers could access to find clues to his or other diseases.
“That is my data, much like an X-ray,” Deutsch said, adding that it belongs to him to share with anyone he likes.

Myriad, which had previously refused to release the data, gave it to the patients the day before the complaint was filed. But the ACLU has said that it regards the complaint as an open matter and wants the agency to make clear that the company has to release complete information when asked by all patients. Myriad spokesman Ron Rogers said the timing of the letters was a coincidence, and the company considers the matter closed.
related video: Should This Fast Company Editor Take 23AndMe’s Spit Test?
This report was produced with support from the National Institute for Health Care Management Foundation.
This article originally appeared on The Eye and is reprinted with permission.
Fast Company , Read Full Story
(50)